The Evidence Based Chiropractor Blog
Hundreds of chiropractic marketing and research articles to help you grow.
Archive
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- October 2022
- July 2022
- May 2022
- March 2022
- February 2022
- October 2021
- January 2021
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- February 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- August 2017
- July 2017
- February 2017
- November 2016
- October 2016
- September 2016
- August 2016
- February 2016
- December 2015
- November 2015
- October 2015
- September 2015
- July 2015
- April 2015
- February 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
The Future of Low Back Pain Clinical Standards
The recent Low Back Pain Clinical Care Standard released by the Australian Commission on Safety and Quality in Health Care underscores a pivotal shift in how low back pain (LBP) is understood and treated in clinical settings.
This standard aims to enhance the quality of patient care and allows chiropractors to align their practices with the latest evidence-based guidelines.
As the leading cause of disability worldwide, low back pain affects millions, costing the Australian health system approximately $4.8 billion annually and impacting the productivity of our workforce significantly.
It’s time for chiropractors to embrace this new paradigm, ensuring their practices evolve with these advancements.
Understanding the Clinical Care Standard
At the forefront of this transformation is the Low Back Pain Clinical Care Standard, designed to provide actionable guidance for the early management of acute episodes of low back pain. Unlike traditional clinical practice guidelines, which cover a broad range of treatment modalities, this standard focuses on key areas requiring immediate improvement in care quality.
It underscores the necessity of a thorough initial clinical assessment, including screening for severe pathology and evaluating psychosocial factors that impede recovery. By incorporating these elements into your practice, you can make informed decisions prioritizing patient safety and well-being.
For instance, did you know that around 70% of patients with low back pain can benefit significantly from guided education and advice alone? This statistic highlights the importance of educating patients about their conditions, addressing fears, and encouraging self-management and activity as part of the initial care approach.
By fostering an environment where patients are encouraged to stay active, you are not just alleviating pain but empowering them to take charge of their health.
Innovative Approaches to Management
The standard calls for a dramatic shift in chiropractic strategies, particularly in the application of imaging and the prescription of pain medications.
With evidence showing that routine imaging does not improve outcomes for most patients, chiropractors should be wary of recommending it without clear justification. Instead, they should focus on comprehensive evaluations to identify those needing further investigation.
Moreover, the standard advises a reasonable approach to pain medications, advocating their use primarily to facilitate physical activity rather than eliminate pain.
Practitioners should prioritize interventions that foster active engagement with care, such as physical and psychological therapies tailored to overcome identified barriers to recovery. This holistic approach enhances treatment effectiveness and aligns with the growing emphasis on collaborative care models.
The Call to Collaborative Action
Integrating the Low Back Pain Clinical Care Standard into your practice is not merely necessary; it is an opportunity to elevate patient outcomes and redefine how low back pain is managed across Australia. As chiropractors, you have a crucial role to play in this initiative. By committing to continuous learning and adapting to new care models, you can provide exemplary patient service that meets the healthcare system’s evolving needs.
Additionally, by collaborating with other health professionals and understanding their roles through the lens of the Clinical Care Standard, you can help create a seamless patient care experience. Communication and teamwork among healthcare providers will enable a multidisciplinary approach to enhance significant recovery for individuals suffering from low back pain.
The Low Back Pain Clinical Care Standard is a rallying point for improving care quality and operational effectiveness in treating low back pain.
Incorporating these principles into daily practice can drive significant improvements in patient care and professional satisfaction, ensuring that chiropractors are seen as vital contributors to the management of low back pain in the healthcare ecosystem.
You can find the full research article here to explore the study further.
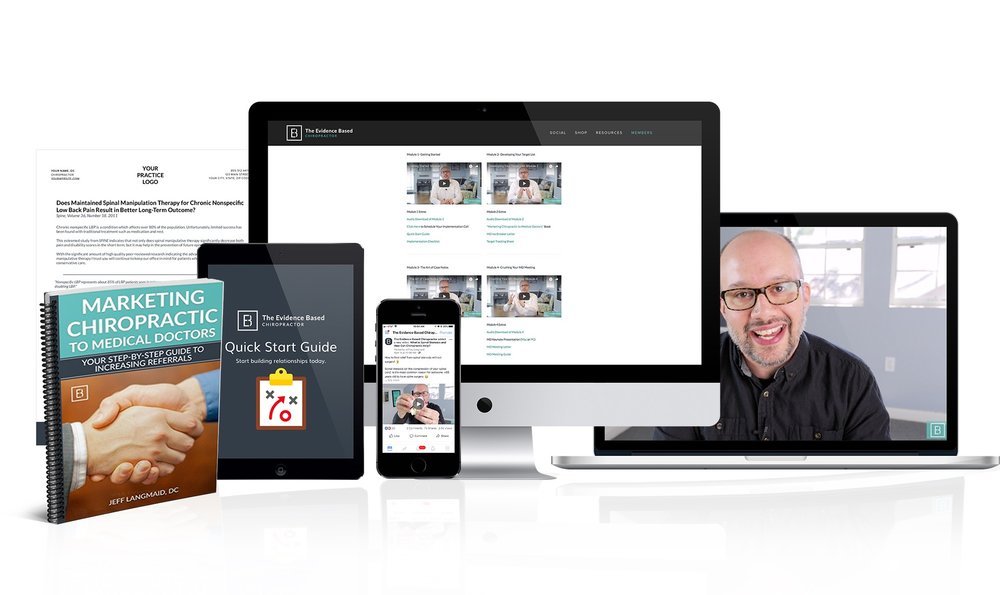
Use Research Like This to Get More Referrals!
Want to get better results faster using a proven referral-building system?
Don't miss out on our proven MD Connection Referral Program, specifically designed to help chiropractors like you build successful referral relationships with medical doctors. The proven program includes everything you need to generate referrals for your practice.
"I've only been a member two days, and I got my first referral from a medical doctor."
- Dr. Bryan Call
"I am currently averaging 30 referrals a month from local providers. Thank you for your help in making this happen!"
- Dr. Boyle
Effectiveness of Spinal Manipulation and Self-Management Compared to Medical Care for Back Pain
Chronic low back pain (cLBP) has become a significant healthcare concern across the globe, affecting millions of individuals and putting immense pressure on healthcare systems.
Recent research underscores the urgent need for practical, non-pharmacological treatment alternatives, especially in the context of the ongoing pain management crisis.
This article delves into the pivotal findings from the PACBACK trial focused on the effectiveness of spinal manipulation therapy (SMT) and supported self-management (SSM) compared to traditional medical care.
Chiropractors play an essential role in delivering these treatments, and with these insights, they can significantly enhance patient care.
The Scale of Low Back Pain
Statistics reveal that low back pain is not only the most common chronic pain condition but also a leading cause of disability worldwide.
Research shows that approximately 20% of acute cases progress to chronic pain, a concerning statistic that drives the need for effective early interventions.
Furthermore, chronic low back pain incurs costs ranging between $560 billion to $635 billion annually in the United States alone. As practitioners dedicated to alleviating pain, chiropractors must prioritize understanding the biopsychosocial elements contributing to low back pain in patients.
The Role of Non-Pharmacological Treatments
Current therapeutic approaches often emphasize pharmacological treatments, leading to a cycle of dependency on medications such as opioids, which can have devastating side effects.
The PACBACK trial presents compelling evidence that non-pharmacological options, like SMT and SSM, can offer substantial benefits without medication risks. Results from this extensive study indicate that integrating these two forms of intervention can foster enduring pain relief and functional improvements for at-risk patients.
Chiropractors are well-positioned to implement these practical strategies, addressing the physical, psychological, and social factors that affect patient outcomes.
Bridging the Gap: Implementation and Effectiveness
The PACBACK trial is a landmark study that examines the effectiveness of targeted interventions for individuals at moderate to high risk of developing chronic low back pain. It employs a robust methodology, enhancing efficacy and implementation strategies within clinical settings.
The future of low back pain management lies in elevating non-pharmacological treatments to the forefront of patient care. By championing spinal manipulation and self-management approaches, chiropractors can transform patients' lives, ushering in a paradigm shift in low back pain management.
You can find the full research article here to explore the study further.
Use Research Like This to Get More Referrals!
Want to get better results faster using a proven referral-building system?
Don't miss out on our proven MD Connection Referral Program, specifically designed to help chiropractors like you build successful referral relationships with medical doctors. The proven program includes everything you need to generate referrals for your practice.
"I've only been a member two days, and I got my first referral from a medical doctor."
- Dr. Bryan Call
"I am currently averaging 30 referrals a month from local providers. Thank you for your help in making this happen!"
- Dr. Boyle
Exploring the Evolution of Scoliosis Treatment
As chiropractors, staying abreast of treatment trends can significantly enhance clinical decision-making and patient outcomes.
Recent research highlighted in the article "Alternative and Adjunct Treatments for Scoliosis" provides a compelling look at how public interest in adjunct treatment methods, particularly chiropractic manipulation, frequency fluctuates about scientific publication trends.
Utilizing tools like Google Trends helps practitioners like yourself assess the growing demand for various treatments, enabling you to effectively tailor conversations and recommendations during patient encounters.
Understanding Public Interest in Chiropractic Manipulation
The analysis from Laubach et al. reveals a discernible upward trajectory in public interest towards chiropractic manipulation as a treatment for scoliosis, with a statistically significant correlation (p < 0.001) between search frequency on Google and time.
This demonstrates a clear opportunity for chiropractors to seize the moment and expand their roles in patient management for scoliosis. As a practitioner, embracing the growing popularity of chiropractic treatment means familiarizing yourself with the latest evidence supporting its efficacy.
It's crucial to explain to your patients that although the interest is high, the scientific literature is still developing, with limited case studies available.
A key statistic from the research indicates that while chiropractic manipulation sees significant interest, detailed research is sparse, making it imperative to remain vigilant in your educational pursuits.
The study underscores a pivotal concern: while public interest may rise, the quality and availability of empirical evidence do not always keep pace. For example, the article notes that chiropractic manipulation is predominantly supported by anecdotal evidence and small observational studies, with limited controlled research available.
This disparity suggests an urgent need for chiropractors to advocate for publishing high-quality studies that comply with robust scientific standards. By doing so, you can contribute to the validation of chiropractic treatment efficacy in adolescent idiopathic scoliosis and enhance your authority as a trusted healthcare provider.
Moreover, when discussing treatment options with parents and patients, emphasize the importance of evidence-based recommendations. Providing insights into how treatments like Schroth exercises and physical therapy also receive attention in the literature can create a well-rounded approach.
Notably, Schroth exercises have been supported in academic literature as effective adjunct treatments for scoliosis, which opens dialogues about multi-modal therapy strategies.
Understanding the seasonal dynamics of interest in scoliosis treatment can provide valuable insights for your practice. The research indicates that chiropractic manipulation and yoga practices show heightened interest during summer and winter, reflecting greater public awareness during periods often associated with physical activity.
As a chiropractor, you can leverage these trends to initiate patient dialogues about scoliosis treatment options during routine visits. This proactive approach demonstrates your commitment to patient education and positions you as a thought leader in a space between popular perception and scientific inquiry.
You can find the full research article here to explore the study further.
Use Research Like This to Get More Referrals!
Want to get better results faster using a proven referral-building system?
Don't miss out on our proven MD Connection Referral Program, specifically designed to help chiropractors like you build successful referral relationships with medical doctors. The proven program includes everything you need to generate referrals for your practice.
"I've only been a member two days, and I got my first referral from a medical doctor."
- Dr. Bryan Call
"I am currently averaging 30 referrals a month from local providers. Thank you for your help in making this happen!"
- Dr. Boyle
The Critical Role of Hip Strength in ACL Injury Risk for Athletes
As chiropractors, our focus is not just on treating injuries but also on preventing them. A recent study has illuminated a pivotal aspect of injury prevention: the connection between hip muscle strength and the risk of noncontact anterior cruciate ligament (ACL) injuries in athletes.
With ACL injuries being some of the most common yet debilitating injuries in sports, understanding and utilizing this information can significantly enhance our approach to patient care.
The Link Between Hip Strength and Noncontact ACL Injury
The study on 501 competitive athletes revealed that diminished hip strength potently predicts future noncontact ACL injuries.
Athletes exhibiting lower isometric hip external rotation and abduction strength showed a substantial increase in injury risk.
The findings indicated that for each unit decrease in hip external rotation strength, the odds of sustaining a noncontact ACL injury increased by 23%, while for hip abduction, the risk was up by 12%.
These statistics unequivocally emphasize the importance of screening for hip strength in our assessment protocols.
The annual incidence rate of noncontact ACL injuries was 3.0%, with separate breakdowns showing 2.5% in males and 4.3% in females.
As practitioners, we must advocate for rigorous pre-season screening, using a clinical cutoff of 20.3% body weight for hip external rotation and 35.4% for hip abduction strength to identify athletes at high risk. These screening measures can help classify athletes into high-risk and low-risk groups, enabling targeted interventions that could reduce injury occurrence.
Screening and Intervention Strategies for Chiropractors
Incorporating hip strength assessments into routine evaluations should become a standard practice for chiropractors working with athletes. Not only does it provide valuable insights into an athlete’s readiness and risk levels, but it also opens the door for proactive treatment options.
For instance, clinicians can develop tailored rehabilitation and strengthening programs targeting these areas if an athlete has weak hip muscles. Strengthening the hip abductors and external rotators can enhance overall lower extremity stability, promoting proper biomechanics during dynamic activities.
Research suggests that interventions to improve hip strength can lead to better movement patterns during athletic activities, reducing the risk of injuries.
In our clinical settings, educating athletes about the importance of hip strength maintenance is crucial. Offering workshops and resources that target lower extremity strength and stability can empower athletes to take proactive roles in their injury prevention strategies.
Integrating these findings into our clinical decision-making empowers us as practitioners and significantly enhances patient care. By prioritizing hip strength assessments, we take vital steps in understanding injury risks, enabling timely interventions, and ultimately fostering healthier, more resilient athletes.
Adopting a preventative mindset is not just beneficial—it's essential for the future of athletic health care.
You can find the full research article here to explore the study further.
Use Research Like This to Get More Referrals!
Want to get better results faster using a proven referral-building system?
Don't miss out on our proven MD Connection Referral Program, specifically designed to help chiropractors like you build successful referral relationships with medical doctors. The proven program includes everything you need to generate referrals for your practice.
"I've only been a member two days, and I got my first referral from a medical doctor."
- Dr. Bryan Call
"I am currently averaging 30 referrals a month from local providers. Thank you for your help in making this happen!"
- Dr. Boyle
The Psychosocial Impact of Chronic Low Back Pain
Chronic low back pain (CLBP) remains a leading global health concern, with significant implications for patient care and clinical decision-making.
Research, such as the qualitative study conducted by Ampiah et al. (2023), has highlighted the multifaceted psychosocial impacts of CLBP among patients in Ghana.
It revealed five critical categories of adverse experiences: loss of self and roles, emotional distress, fear, stigmatization, and marginalization, along with the crucial role of social support.
As chiropractors, understanding these components is vital for enhancing clinical approaches and patient outcomes.
Understanding the Loss of Self and Roles
The loss of self-experience significantly influences how patients cope with CLBP. Participants in the study articulated feelings of incapacity and fragmentation of identity, often stemming from the pain that alters their daily lives.
Statistics suggest that around 34% of Ghanaian adults experience low back pain, highlighting the urgent need for intervention.
Chiropractors should prioritize addressing physical pain and supporting patients’ emotional and psychological needs. This may include fostering resilience through education and empowering patients to redefine their roles within their families and communities.
Emotional Distress and Support Mechanisms
Emotional distress is a robust predictor of chronic pain outcomes. The study reports that participants frequently experienced anxiety and frustration related to their condition, leading to feelings of helplessness.
This psychological burden is compounded by fears of long-term disability, often exacerbated by healthcare professionals' biomedical orientations.
As chiropractors, it is essential to adopt a biopsychosocial approach, acknowledging these emotional components alongside physical treatment.
Providing a supportive environment that encourages open communication can mitigate the adverse effects of distress.
Access to support resources, such as counseling or peer support groups, can also enhance patient care.
Implications for Clinical Practice
The findings from Ampiah et al. emphasize the necessity for chiropractors to reassess their management strategies for patients with CLBP.
Incorporating psychosocial factors into treatment plans is paramount. Strategies should emphasize patient education regarding the nature of pain, addressing misconceptions, and promoting active coping strategies rather than passive ones.
Moreover, fostering partnerships with family members can enhance support networks for patients suffering from CLBP, thereby improving outcomes.
You can find the full research article here to explore the study further.
Use Research Like This to Get More Referrals!
Want to get better results faster using a proven referral-building system?
Don't miss out on our proven MD Connection Referral Program, specifically designed to help chiropractors like you build successful referral relationships with medical doctors. The proven program includes everything you need to generate referrals for your practice.